“It’s not good enough.”
I hear it or read it every week.
It is *insert time frame here* days/weeks to see a GP.
It’s not good enough.
Sometimes it is 6 days, 16 days, 6 weeks.
I totally understand. I would like to see a 1-2 week wait to be the maximum anyone has to wait to speak to a GP. I have kids, I have a mum in her 70s. I want to be able to trust the NHS to be there just when we all need it.
Being able to see people in the timeframe of their choosing would also make my job a lot easier and a lot more enjoyable (wouldn’t ever start the consultation “Doc, it’s been a while”, or “do you know it’s taken me 42 days to see a GP… “not on the golf course today Doc?” etc etc). A lot of people do come in and say “I know you are busy”. And I think overall, patients are understanding (not that you would think this when you look at most GP practice Google reviews).
Everyone has a different threshold for what isn’t good enough depending on their previous experience of trying to get a GP appointment. e.g. 15 years ago it was pretty simple getting an appointment on the day or certainly within 2 weeks time. People also have different thresholds for what is OK depending on how they are feeling. Understandably, patients are scared/worried about their symptoms and this anticipation of the wait just adds to the feeling of unwellness (not sure that is a word but if wellness is….).
So why is the NHS making us all wait?
Ambulance wait times have expanded, where you could expect a category 2 (sepsis, stroke) ambulance in 18 minutes, many patients are waiting 2-3 hours+. We are waiting 4-5 hours for ambulances to attend for possible asthma attacks in surgery.
A&E wait times have grown significantly, you might wait 12 hours to be assessed for abdominal pain or breathing difficulties (if not life threatening emergency).
Hospital clinic waits have also extended. Locally, urgent dermatology can be up to a 6 month wait for clinic review, a 12-18 month wait is normal for a routine neurology referral, and an 80 week wait for a routine colonoscopy is to be expected.
Is this just because there are more people waiting?
I wish it were that simple.
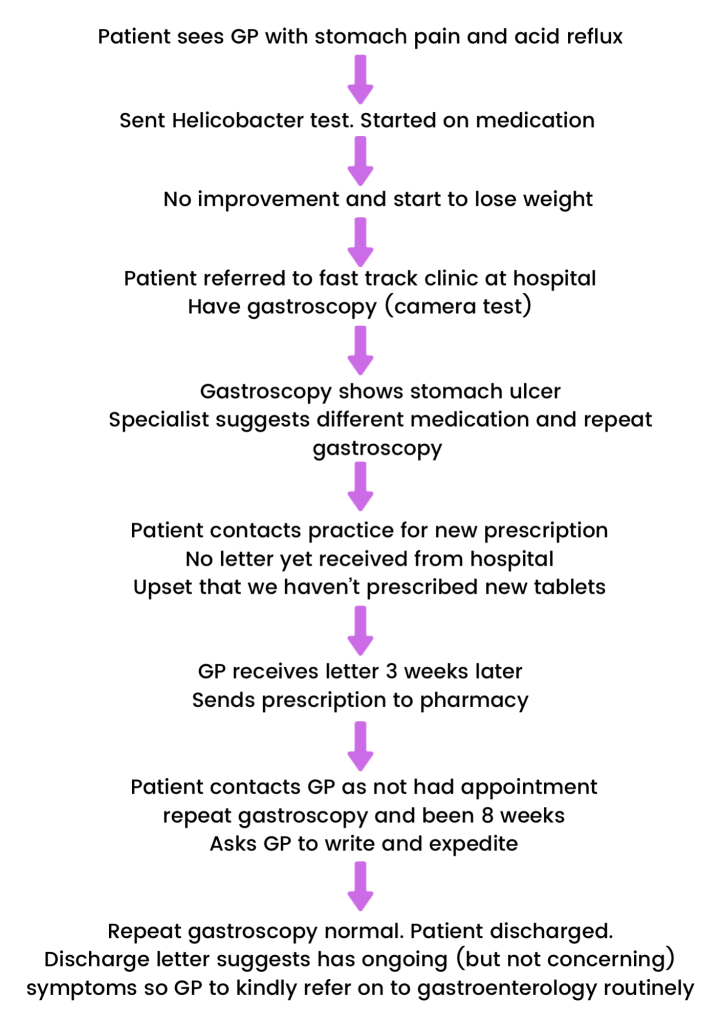
Yes, there are more people seeking care. There are also problems with “flow”. I hate the term flow when it is applied to people and patients, but sometimes needs must. It would be lovely if, when I referred a patient to clinic for abdominal pain, it would be a full holistic review. The patient arrived at clinic unsure about their symptoms and was discharged with answers and resolution of their symptoms.
As a GP, I do all the tests and treatments I can and then I refer on for specialist input where appropriate. In an ideal world, the specialist would offer a full assessment and consider all causes of the patient’s symptoms. They would have time to explain the diagnosis, treatment plan and arrange timely follow up.
Sadly, we have moved to a more test-based system. Test is normal, discharge back to GP. Refer on to another specialist. Their test normal. Discharge to GP and so on.
Have we lost sight of the whole person?
More about flow…
The flow of patients admitted to hospitals can be slow. A&E waits are often due to the department being full of patients awaiting beds. Hospital wards are often filled with patients awaiting social care so they can safely return home. GP appointments are often filled with patients who have queries about treatments provided by the hospital or who are awaiting hospital specialist clinic appointments.
When a patient is referred to a specialist clinic, they might wait 3 months or 3 years depending on the area and speciality. That patient doesn’t just sit at home waiting. No, they rightly come to us for ongoing support of their pain, constipation or anxiety.
What does that mean for GP practices?
Routine GP waits have extended to 2-6 weeks depending on where you are in the country. Many practice still see a huge proportion of patients with urgent problems on the day (or within 24 hours of patient contact).
We fill our “on the day/urgent” appointments by lunchtime every day. We have a waiting list for patients who have ongoing/non-urgent symptoms. This waiting list can be anything from 2-8 weeks depending on staffing and demand.
Surely you just need to employ more GPs?
More GPs. More appointments.
Yes, wouldn’t that be lovely.
Sadly, funding for GP practices has fallen year on year since I first started GP training in 2010. Practices are being squeezed and just cannot afford to bring on more GPs.
We need to look at the whole system, not just GP practices
This isn’t an us (GPs) vs them (hospital doctors). It is difficult for every sector of the NHS at the moment. I can only comment on the part of the system that I work in.
So many of my appointments are used by patients who are understandably frustrated by waiting for some form of test or intervention elsewhere in the NHS. Some of my appointments are taken us by patients who have been told to get in touch with the GP by a specialist.
If you have been to a hospital clinic or discharged by a ward recently, you might have seen “actions for GP” on the letter. These actions take us time. We are working with our local hospitals to try and ensure only appropriate things come to the GP to do. We are not here to do the work of our hospital colleagues: prescriptions, sick notes, arrange post-op dressings etc, they can all be arranged by hospital clinicians. I want to be spending my time looking after my patients, not being asked to do more and more administrative tasks.

I want to help more patients, reduce the waiting list. I want to be able to see all the people that want to come and see me and need the care of a GP. But sadly there is a mismatch of appointments and number of patients wanting them.
Other factors
I think we are living in an “amazon prime” generation. People get sick, they contact us and want quick answers. They can get their rechargeable handwarmers they ordered earlier today at 10pm tonight (can you tell I am freezing my hands off on the sidelines as a football mum?), so why not advice within 6 hours from a GP. There is no blame here, times are a changing and we (the NHS) need to move with the times.
People are also living longer, but with more complex healthcare needs. It is important we offer these patients the time and care they need. Mental health illness is impacting more people. Mental Health services (adults and children) are struggling to keep up with this need. GPs are important to the care and support of vulnerable patients.
The lack of investment and funding in general practice has lead to buildings that aren’t fit for modern healthcare. Practices have recruited more clinical staff (addition of pharmacists, physios, social prescribers etc in recent years via the ARRS scheme).
With expansion of medical schools and GP training programs, we also need to find space for more trainees and students. It is difficult to fit everyone in traditional practice premises. We just don’t have the space or funds to make more room (modernisation/extension/new build) or to hire more staff.
We cannot keep trying to do it all.
There is a finite resource. There are a certain number of appointments and a larger number of patients needing them. The waiting rooms aren’t empty, the clinics are full – we are just better at making sure you don’t need to wait,
Does the NHS need to separate out patients who want quick advice (eg about their cold symptoms or UTI) vs those that want long term continuity or have more complex healthcare needs?
I often see patients in my surgery who have had a cough for 3 days or a child with a temperature for 6 hours. At times I wonder if we are too accessible. Later on I will see a patient with weight loss and swallowing difficulties that maybe waited 11 days and should have been seen sooner.
I think NHS leaders have a duty to explain to patients what they can currently expect from the various parts of the NHS with the funding that we receive.
How can you help?
Consider when you need to speak to a GP or a clinician. Could you attend your local pharmacy instead? Could you check your symptoms on the NHS website first?
Many problems get better within 3-4 weeks. It can feel worrying waiting, but a lot of patients end up cancelling their pre-booked appointments as their symptoms have resolved.
As a GP partner, I need to make sure the precious resource of a GP appointment goes to the most in need. This means I might sign post you to your local pharmacy if you have symptoms of a minor illness.
Stock up on remedies for common symptoms of viral illness eg pain relief and decongestants. Accept that many viral illness take 5-10 days to resolve. I know you feel rubbish, I know you need to get back to work. I know you have kids to look after. Antibiotics aren’t going to make any of those things better.
NHS111 might have a better role here. To help sign post patients to the most appropriate NHS service. It’s certainly not perfect at the moment but it’s heading in the right direction.
Do we (the NHS as a whole) need to educate children in schools, parents, carers etc about viral illness and when to seek help? Rather than the “if something doesn’t feel right” adverts, I would prefer to see “your child has a temperature, what to expect and how to help” adverts.
Understand why your GP might say no. Practices aren’t funded to do everything and anything. Read more here in my Collective Action blog post.
Is the wait for a GP appointment going to continue?
Yes. Until General Practice is funded and resourced properly, we will continue to work in this way. We have to balance the need for same-day urgent appointments, vs trying to keep the wait for routine appointments as low as possible.
GPs are also leaving because the job is stressful and unsustainable.
Maybe the new GP contract in April will bring more much needed funds to General Practice?
We need to work in buildings that are fit for purpose. We need more GPs and more nurses. We need the job to be fulfilling to stop GPs leaving the profession.
We shall see.
I can guarantee your GP is trying really hard.
If they have offered you excellent care, leave them an NHS or Google review or send a card/email saying thanks. Little things like this, really lift the whole practice.
Support your practice. Write to your MP.
We know that high quality general practice and continuity of care saves lives. Let’s safeguard this for our own future, and that of our loved ones.

My GP practice is brilliant, often get an appointment on the same day if urgent otherwise within 2 days unless wishing to see a specific GP.
LikeLiked by 1 person